
New E/M Coding Guidelines for Optometrists
In 2021, CMS (Center for Medicare and Medicaid Services) changed their old 1995/1997 E/M coding rules to allow doctors to document their visits based on medical decision-making (MDM) or time alone. Although still an essential and required part of every office visit, patient history and physical exam elements were completely eliminated from the E/M coding process. The intent of these changes was to increase the doctor’s focus on patient care by reducing documentation for the purpose of achieving a certain E/M level.
In 2023, the AMA (American Medical Association) released their CPT revisions to the E/M coding guidelines to further reduce administrative burden. CMS adopted some of those revisions but not all.
This article summarizes these significant 2021/2023 changes to E/M coding and provides some guidance navigating the new coding rules.
MDM or Time: Which one?
With the new E/M guidelines, doctors can code their medical exams based on MDM or time. Given an option, which one should you choose? There is not one right answer. It really depends on the specialization and needs of your practice. Let’s explore both options so you can make an informed decision.
MDM
The new MDM requirements put a larger focus on patient care rather than documentation. Whereas before doctors had to document patient history and physical exam to code E/M, they are now asked to perform and document clinically important tasks that directly contribute to managing a particular condition. Of course, that does not mean that you don’t have to document the patient’s history anymore or perform the exam. You still do; however, only to the extent that it helps you manage the patient’s condition. That gives doctors more freedom to determine what they deem relevant and eliminate tasks which before were solely performed to meet E/M coding rules.
The 2021 E/M changes introduced these 3 elements to medical decision making:
- Number and complexity of problems (diagnoses) addressed
- Amount and/or complexity of data to be reviewed and analyzed
- Risk of complications and/or morbidity or mortality
There are 4 levels of MDM: straightforward, low, moderate, and high. Below table summarizes the AMA’s scoring system for MDM as it pertains to office visits.
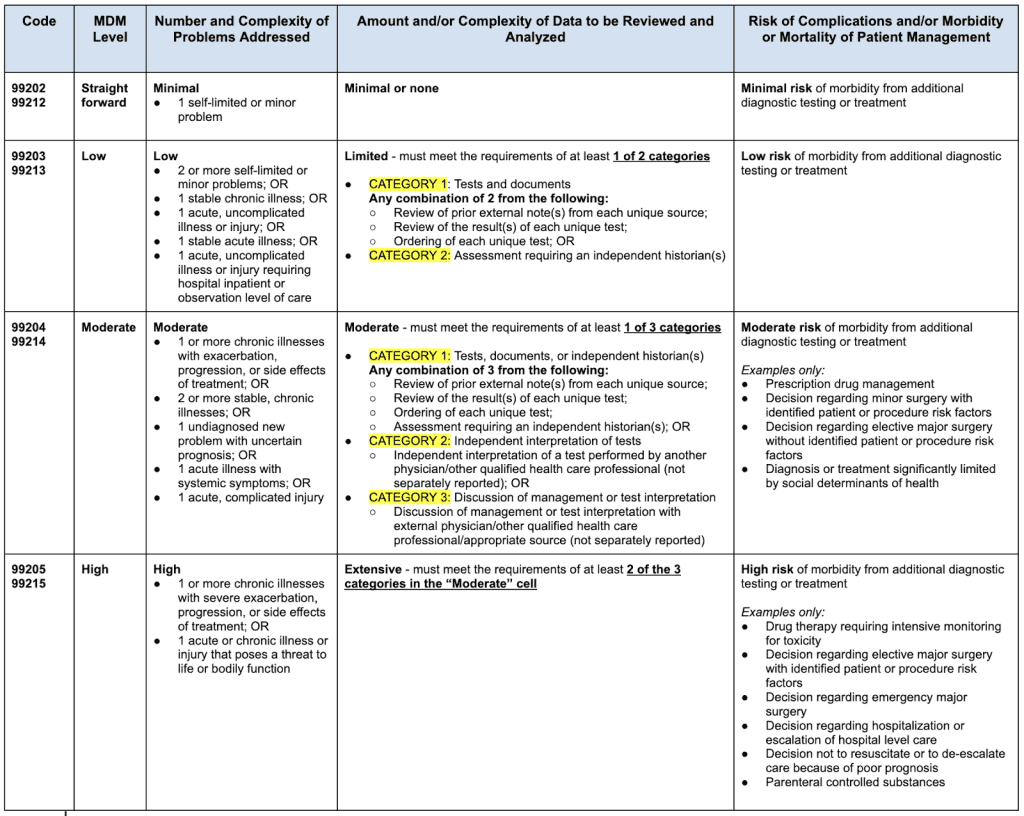
Notes:
- CPT ® code 99201 (new patient, level 1) was deleted.
- CPT ® code 99211 can still be used for a minimal problem, where the presence of the doctor or other qualified healthcare professional may not be required; however, patient care is provided under the doctor’s or other qualified healthcare professional’s supervision.
At first glance, the above scoring grid might look quite extensive, especially in the data column. However, there are really only 6 data tasks that are combined into different categories based on MDM level. Let’s take a look at those 6 data tasks to define and clarify a few points.
- Review of prior external note from each unique source.
- Review of the results of each unique test.
- Ordering of each unique test.
- Assessment requiring an independent historian.
- Independent interpretation of a test performed by another physician/other qualified healthcare professional.
- Discussion of management or test interpretation with external physician/other qualified healthcare professional/appropriate source.
Definitions:
What defines an “external note”?
An “external” note can be health care records and/or communications from another doctor, qualified healthcare professional, facility, or healthcare organization who/which is not in the same group practice, or is of a different specialty or subspecialty. So, if you are an OD reviewing patient notes from an ophthalmologist who works in the same practice as you, this data criteria would be met.
What is a “unique source”?
A unique source is defined as a doctor or qualified healthcare professional in a distinct group or different specialty or subspecialty, or a unique entity.
What is a “unique test”?
“Unique” in this case is defined by a CPT code. When multiple results of the same unique test (e.g., serial IOP readings) are compared, count it as one unique test.
What is an “independent historian”?
An “independent historian” is a person (parent, guardian, surrogate, spouse, witness) who is able to provide the patient’s medical history in the case where the patient is unable to provide a complete or reliable history themselves (due to developmental stage, dementia, or psychosis).
Clarification:
- Keep in mind that reviewing all notes from any unique source counts as one element toward MDM.
- The review of a test is inherent in the order; so, don’t count reviewing separately into MDM if you also ordered the test, whether the review is done the same day or in a subsequent encounter.
- Tests that do not require separate interpretation (tests that are results only) may be counted as ordered or reviewed (not both) for selecting an MDM level. They do not count as an independent interpretation.
- The ordering and actual performance of diagnostic tests cannot be counted towards MDM if the professional interpretation of those tests is reported separately.
- If your same specialty partner in your practice reported the professional component, do not credit an independent interpretation when you see the patient.
- A form of interpretation should be documented but need not conform to the usual standards of a complete report for the test.
- As for assessments requiring an independent historian, note that the history may be provided in person, through writing or electronic means (email, patient portal etc.).
Now that you have a better understanding of the different MDM levels and their documentation requirements, let’s discuss how to determine the billable E/M code based on those requirements.
Determining the Final E/M Code
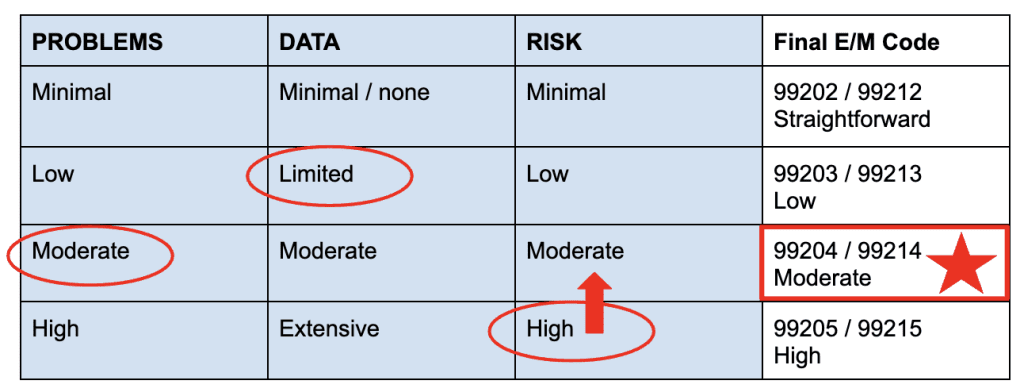
To qualify for a particular level of MDM, two of the three elements for that level of MDM must be met or exceeded. The “E/M Decision Grid” table below summarizes the three elements (problems, data, and risk) with their four MDM levels (straightforward, low, moderate, and high).
If you scored the same level in all three or two elements, then your final E/M code is clear. If, however, you scored a different level in each element, then you should reference the middle score level and lower the highest score level down to that same middle level in order to achieve two elements (see example below). You should not bring a lower score level up to a higher level since you would be over-coding your exam.
E/M Decision Grid:
MDM Summary
In summary, this is how the new MDM coding works. It does require a clear understanding of the documentation requirements in order to avoid under or over-coding. However, if you have studied the requirements and find yourself performing most of the data tasks on a regular basis, then MDM based E/M coding might be the right method for you. Otherwise, there is always the option of time-based E/M coding. Let’s explore this option next.
Time
As an alternative to billing by MDM, you can bill based on the amount of time you spend working on an encounter. With the previous E/M guidelines, you could only bill for time that you spend face-to-face with the patient. With the new 2021/23 guidelines, time is defined as the total time spent on a given encounter. The following activities add to the total time, when performed:
- preparing to see the patient (e.g., review of tests)
- obtaining and/or reviewing separately obtained history
- performing a medically appropriate examination and/or evaluation
- counseling and educating the patient/family/caregiver
- ordering medications, tests, or procedures
- referring and communicating with other health care professionals (when not separately reported)
- documenting clinical information in the electronic or other health record
- independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver
- care coordination (not separately reported)
Here are a few important points to consider when documenting based on time:
- Activities that count toward time must be performed by one, or multiple, doctors or other qualified healthcare professionals on the same day as the patient visit. That is, if you continue to work on the patient’s chart on another day you cannot count the time spent on that day towards the visit.
- The time must be spent by the doctor/qualified healthcare professional. Do not count staff time.
- If more than one doctor/qualified healthcare professional spends time on the encounter you can add up their time, but only if they do not work on a particular task together, or at the same time. Meaning, if it’s time spent collaboratively, only count the time spent once.
- If you bill for an activity separately then that activity cannot be counted towards time.
- If you decide to bill based on time then document the activities and total time spent in the chart. For example: “I spent xx minutes seeing the patient, performing a vision wellness exam, coordinating care with a cataracts specialist after diagnosing early stages of cataracts and documenting the record.” The AMA in their CPT rules does not require practitioners to list out how much time they spent on each task but some private payers might. So, be sure to double check if in doubt.
The table below shows which E/M code can be billed for the different time ranges (in minutes).
E/M Code | Total Time Spent |
99202 | 15-29 |
99203 | 30-44 |
99204 | 45-59 |
99205 | 60-74 |
99212 | 10-19 |
99213 | 20-29 |
99214 | 30-39 |
99215 | 40-54 |
Conclusion:
The 2021/23 E/M coding changes allow for more flexibility in documenting office visits. Hopefully, this will avail you to spend more quality time with the patient and reduce your charting efforts.
Both coding based on MDM and time have their pros and cons. MDM is more likely to get you to a higher E/M code than time for the typical visit; however, MDM requires the doctor to be closely familiar with the documentation guidelines in order to avoid under or over-coding. Time is easy to implement and document; however, it may also result in a lower E/M code unless the visit is excessively long.
So, which one should you use: MDM or time? Depending on the specific visit, you might decide to code one medical exam based on MDM and another one with time. If you see the patient for a regular exam, you might be better off using MDM to achieve a higher E/M code. If, however, you are dealing with a complex care scenario that significantly extends the time you spend with the patient, consider billing by time. Either way, it is best to only document the method you want to use for billing (i.e., the one that will pay you more) instead of both. For example, if time gives you a 99202 but MDM gives you a 99203, then only document for MDM and do not document how much time you spent. Why? Because if you get audited, the insurance companies will always go by the documentation that pays you less.
Online Scheduler
Patients can easily find their doctors and schedule appointments online. Patients benefit by having access to their doctor’s live schedule and staff members benefit by being able to prioritize other important tasks in the office.
Learn moreAdvanced Scanning
EyePegasus features an effective scanning solution aimed at doctors who are currently looking to efficiently and securely digitize their existing paper charts. In addition, day-to-day scanning needs are also supported.
Learn moreTwo Ways SMS
Stay in touch with your patients, improve communication and increase overall patient satisfaction. With two-ways text messages you can keep context of your conversations and reach your patients efficiently.
Learn more